
Low Back Pain & Sciatica
Low back pain is a very common problem that affects at least 80 percent of all individuals at some point in their lifetime. It is also a frequent reason for physician visits,[1] and causes more disability worldwide than any other condition.[2] Indeed, low back pain is the leading cause of work absence in much of the world.[3] A large majority of these individuals recover within a few months; however, some will have recurring episodes[4] or may even develop chronic—perhaps even constant—low back pain.[5] In the United States, it is estimated that more than five million people are disabled—not just troubled—by low back pain, half of whom are permanently disabled.[6] Despite advanced medical technology, the number of patients suffering from low back pain continues to increase.[7]
Common Causes of Low Back Pain
Low back pain can be acute (meaning it comes on suddenly and lasts for only a short time) or chronic (meaning it tends to come on slower and lasts longer than three months). It can appear after a sudden trauma or injury, but also may seem to appear suddenly after an innocent cough or small movement. In those cases, it had been accumulating over time—that last small motion was simply “the straw that broke the camel’s back,” as it were. Engaging in a variety of sports activities—gymnastics, football, weight lifting, rowing, golf, dance, tennis, baseball, basketball, and cycling—increases the odds of having low back pain,[8] as do increased age, previous episodes of low back pain, hard physical labor, and poor posture, especially with certain activities—such as lifting or carrying heavy loads. Other contributing factors include mental stress, osteoporosis,[9] joint hypermobility,[10] or, surprisingly, physical inactivity.[11]
There are various causes of low back pain. Most (estimated at 90 percent) low back pain is caused by ligament sprains, muscle pulls, or disc herniations resulting from either overuse or straining, spraining, lifting, or bending.[12] This is known as “mechanical low back pain.” In many cases, the back pain is localized to the back itself; in other cases, the pain may travel into the buttocks or legs as well. Other reasons for low back pain—usually more chronic—include osteoarthritis (OA; inflammation caused by calcium spurs in the joint), central canal stenosis (where the spinal canal has become narrowed because of arthritis or other degenerative changes), facet joint dysfunction (when the joints that connect the vertebrae—the facets—don’t function properly, often because the ligaments connecting them have been injured), and spondylolisthesis (slippage of one vertebrate over another, which can be congenital or a result of trauma). Another, often overlooked, cause of low back pain is the sacroiliac (SI) joint,[13] responsible for causing at least a third of cases of low back pain in one large study.[14]

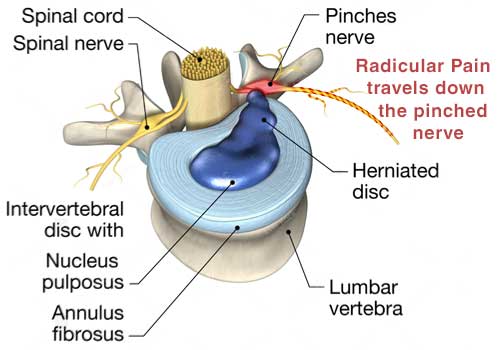
MRIs can be misleading in diagnosing this type of musculoskeletal pain. In 1905, the Boston Medical and Surgical Journal (later renamed the New England Journal of Medicine), published a paper that proposed sacroiliac (SI) joint dysfunction and ligament laxity as being the main generators of low back pain.[15] For the next 30 years, the medical community largely agreed. Then in 1934, the research of William Mixter and Joseph Barr became popular.[16] They focused attention on the intervertebral disc: a circular, collagen-type tissue that sits between the bones (vertebrae) in the spine. From that time forward, attention to “disc disease” overshadowed that given to the SI joint and ligaments. Then the 1970s saw the introduction of CT scanners (computed tomography, a very sophisticated type of three-dimensional X-ray), and the 1980s heralded the MRI—and both have been used readily ever since. It so happens that intervertebral discs are easily seen with both types of scans, which inspired further attention to the disc as being the cause of low back pain.
Understandably, patients—and their doctors—are eager to find the cause of their pain; an abnormality on an MRI provides a seemingly obvious “reason.” But, as a well-respected textbook of orthopedic medicine states, “The results of radiographic examinations should never be given to the patient as a diagnosis.”[17] Medical studies have documented over and over again that what the scan shows may not be the reason for the person’s pain. In fact, although a diagnosis of disc herniation is frequently given as the cause of pain, it has been widely reported that only 4 percent of low back pain is due to a herniated disc.[18] Ligament injury is in fact a more common cause of low back pain,[19] because ligament laxity in the spinal ligaments always precedes disc herniations.[20] The trouble is, ligament injury is difficult to prove with an MRI or CT scan unless the injury is significant, which is usually not the case. And, as discussed earlier, MRI scans require that the patient remain still. However, small ligament or tendon abnormalities may not show up on imaging until the joint is moving, so an MRI may not identify the problem.
This isn’t to discount those who suffer from true intervertebral disc problems, nor to say that MRI and CT scans are useless. It is simply to say that radiographic findings should not automatically be accepted as the cause of pain until other sources have been proven unlikely.[21]
Surgery for Low Back Pain
During recent years, the general public has accepted the idea that a herniated disc requires surgery, especially if the pain has not resolved after a few weeks and there is a positive MRI or CT. However common, this opinion has not been supported by evidence in long-term studies which show, instead, that equally good or better results are obtained after conservative nonsurgical treatment. For that reason, most doctors recommend that conservative treatments should be undertaken first[22], and that a large percentage of the time, disc herniations seen on MRI scans resolve on their own without surgery.[23]
The Sacroiliac Joint
The sacrum is a triangular shaped bone that sits at the bottom of the spine. On each side of the sacrum is another bone called the “iliac bone”. The joint between each side of the sacrum and the iliac bone is therefore called a “sacroiliac” joint (abbreviated “SI”), and all these bones together form the “pelvis”. The pelvis is held together by a large number of ligaments—and where there are ligaments, the possibility of injury and pain exists. In fact, as early as 1905, the SI joint was identified as a significant source of low back and posterior pelvic pain[24].
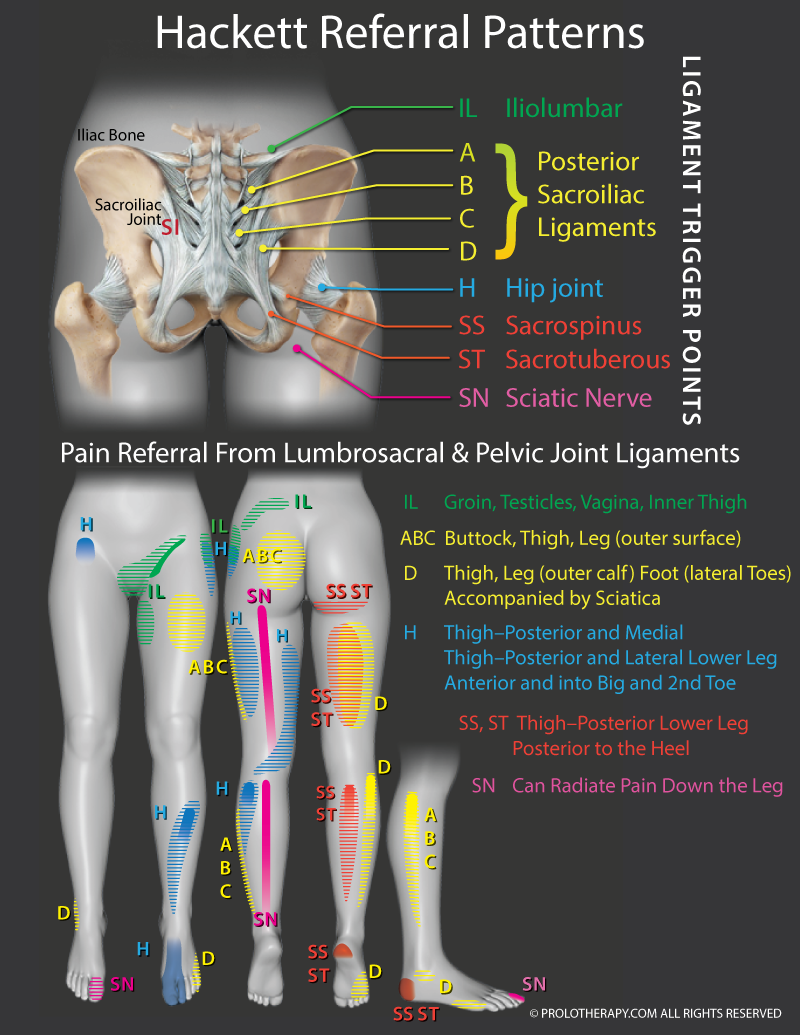
In the last several years, there has been renewed interest in the SI joint as an underappreciated cause of low back pain in patients of all ages.[25] Multiple studies and investigations have also discovered that SI ligament or joint injuries may also “refer” pain into the buttocks, thigh, hip, groin, leg, ankle, and even the foot[26] (remember from earlier that “referred” pain is pain that is felt at a distance from where it is coming from—for instance, when a person is having a heart attack, he or she may feel pain in the left arm, which is being “referred” there from the heart). Sacroiliac injuries can also imitate sciatica[27] (sharp buttocks and leg pain), discussed in the next section. The ability of the body to refer pain from the SI joint and other ligaments in the low back is seen in Figure 1 .
Common Causes of Sciatica
The term sciatica is often used to describe any type of pain that follows the course of the sciatic nerve that runs from the buttocks down the back of the leg. Although the term “sciatica” is descriptive of where the pain is located, it is a general term that does not necessarily convey the cause of the problem. There can be several reasons for sciatica. As mentioned above, a common cause of sciatica is “SI joint dysfunction” or “SI joint instability”. There are several ways instability there can cause sciatica. If ligament laxity develops there, muscles around it spasm in an attempt to stabilize it, and this spasm then puts pressure on nearby nerves running down the leg. Or the excess motion of the sacrum may eventually directly aggravate nearby nerves. Another cause of sciatica is “Piriformis Syndrome”, which can exist all by itself or in combination with SI joint instability. This is not hard to understand when you review the anatomy and how close the SI joint is to the piriformis muscle. If any of these pelvic ligaments are sprained, this swelling will also put pressure on nearby nerves which travel down the leg. Just as a sprained ankle swells after an injury, sprained connective tissue in the pelvis will swell when injured, putting pressure on the sciatic—or other low back nerve roots—causing “sciatica.”
This is especially true when the piriformis muscle and tendons are irritated, because this large muscle runs directly over the large sciatic nerve.
These are very common causes of sciatica. In fact, a large study of 1,293 patients who were followed over a 12-year period of time concluded that SI joint syndromes (and posterior joint syndromes) are the most common referred-pain syndromes, occurring twice as frequently as nerve root compression caused by a herniated disc or stenosis, and they often mimic those symptoms[28]
Fortunately, Prolotherapy can help. A study by Dr. John Merriman compared Dextrose Prolotherapy treatment to lumbar fusion surgery as a treatment for sciatic pain. His conclusion was that 80 to 90 percent of more than 15,000 patients experienced relief from sciatica with Prolotherapy, with far fewer side effects than those patients who had undergone a fusion operation.[29] Other investigations have also confirmed the efficacy of Prolotherapy to resolve sciatica-like symptoms.[30]
Sacroiliac Joint versus True Radicular (Spinal Nerve–Generated) Pain
A (thankfully) much less common source of sciatica results from true nerve root compression—when something is actually structurally pressing against a nerve. Remember, a nerve can experience pressure from a swollen ligament or a spasmed muscle pushing against it, as in Piriformis Syndrome, and this type of nerve compression will get better once the ligament, tendon, or muscle weakness and injury is addressed and resolved. You see, the nerve doesn’t know what’s pressing on it and will respond the same way whether it’s a temporary pressure because of swelling nearby or an actual true nerve root being compressed. True radicular pain, however, is structural in nature and can be caused by stenosis (narrowing of the spinal canal), or a true, active herniated disc or fragment that is pressing on a nerve. Because SI joint pain can imitate the pain that’s generated by true nerve compression, it is important for the doctor to determine the actual cause of the pain. To confuse the issue further, both types of pain can coexist in the same person. It is estimated that 33.5 percent of patients with low back pain have both.[31] But there are certain differences between these two types of pain.
Pain coming from the SI joint is usually deep, achy, and ill defined, and will often feel tender in response to light pressure. There may be muscle weakness from inactivity, but rarely muscle loss (atrophy). There are also a few simple tests to determine if the origin of pain is likely coming from the SI joint. A basic test was proposed in 1960 by Dr. John Mennell: if the patient, when asked where the pain is, “points over one or the other sacroiliac joints, then the cause of the pain probably lies within that [SI] joint.”[32][32] Almost 40 years later, Dr. Joseph Fortin published the “Fortin Finger Test” in the American Journal of Orthopedics. This study involved pushing on the SI joint line to see if it caused any discomfort or pain. If so, a local anesthetic was injected into the SI joint to see if there was any temporary reduction in pain, and if so, chances were that at least some of the problem lay within that SI joint.[33] Fortunately, multiple studies have shown the efficacy of Prolotherapy for SI joint pain.[34]
Radicular (true spinal nerve compression origin) pain, on the other hand, typically involves sharp pain, which can feel “electric.” The patient can have numbness, tingling, burning, or coolness—and sometimes worse pain in the leg than in the back. There may also be actual muscle loss (atrophy) in the leg, in addition to weakness.
As you might imagine, a proper diagnosis for the cause of sciatica calls for both a comprehensive analysis of a patient’s history as well as a thorough physical exam. As long as there are no neurological warning signs, such as loss of bowel or bladder function, profound muscle atrophy, loss of tendon reflexes, unrelenting sharp leg pain inhibiting the ability to walk, or other alarming signs, the doctor may determine that a trial treatment with Prolotherapy is reasonable based on the origin of the problem most likely being primarily musculoskeletal rather than coming from true nerve root compression. However, treatments and progress should be monitored closely to ensure improvement. In a very small number of cases, surgery may be needed to relieve pressure on the nerve if symptoms do not improve with conservative treatment.
How Prolotherapy Regenerative Medicine Helps Low Back Pain
Traditional Dextrose Prolotherapy stabilizes low back, sacroiliac and pelvic ligaments and has been used successfully for these problems for many years.[35] Platelet-rich plasma (PRP) has been found effective for SI joint dysfunction, demonstrating in one study continued pain reduction and functional improvement up to the last patient follow up four years after the treatment.[36] PRP has also been successfully used for lumbar facet joint (the joints between the vertebrae),[37] as well as muscular-based low back pain.[38] PRP has also been compared to a traditional treatment—cortisone—and found to be superior.[39] Biocellular formulas, although newer, have also shown success when used for these conditions.[40]